You’re a PA student on your ER rotation. A patient arrives and your attending sends you to see him and report back.
51 y/o M w PMH of GERD and kidney stones presents to ED with a c/o 8/10 chest pain
- Radiation: positive: left arm, neck, stomach and ear
- Timing: Since 5 am (it’s 9:30am now)
- Character: sharp, stabbing, pressure-like
- Relieved by leaning forward? No
- Pleuritic: No, does not get worse w inspiration
- How did it start? Woke him up from sleep
- Cough, SOB? No
- History of VTE? No
- No fever, chills, vomiting but yes to nausea
- Has never happened to him before
- Has not tried to walk since pain onset so he is unsure if it’s exertional
- Took an antacid and 400mg Tylenol at 7am with no relief
- Denies smoking or alcohol use
- FH: father dies from “heart disease” at age 40
PMH:
- GERD;
- Kidney stones but no lithotripsy or surgery;
- does not know his vaccination status,
- last PCP visit 1.5 yrs ago
PSH: Denies
Medications: Antacid situationally
Allergies: NKDA, NKEA, NKFA
FH: See HPI
SH: J.F.is a single male living alone, denies smoking, use of alcohol, caffeine or illicit drugs. Denies being sexually active at the moment.
ROS:
General: Denies any fever, chills, night sweats, fatigue, weakness, loss of appetite
Skin, hair, nails: Denies changes in texture, excessive dryness or sweating, discolorations, pigmentations, moles/rashes, pruritus, changes in hair distribution
Head: Denies headache, vertigo, unconsciousness, coma
Eyes: Denies photophobia ,visual disturbances, fatigue, lacrimation
Ears: Denies deafness, pain, discharge, tinnitus
Nose/Sinuses: Denies discharge, epistaxis, obstruction
Mouth and throat: Denies bleeding gums, sore tongue, difficulty swallowing
Neck: Denies localized swelling/lumps, stiffness/decreased range of motion
Pulmonary system: Denies dyspnea, SOB, cough, wheezing, hemoptysis, cyanosis, orthopnea, PND
Cardiovascular system: Admits to chest pain as per HPI, denies HTN, palpitations, irregular heartbeat, edema/swelling of ankles or feet, syncope, known heart murmur
Gastrointestinal system: Endorses slight nausea but no vomiting this morning, denies changes in appetite, intolerance to foods, dysphagia, pyrosis, flatulence, eructation, abdominal pain, diarrhea, jaundice, change in bowel habits, hemorrhoids, constipation, rectal bleeding, blood in stool, pain in flank
Genitourinary: Denies frequency, incontinence, dysuria, nocturia, urgency, oliguria, polyuria, hesitancy, dribbling
Musculoskeletal system: Denies Muscle/joint pain, deformity or swelling, redness
Peripheral Vascular system: denies intermittent claudication, coldness of trophic changes, varicose veins, peripheral edema, color change
Hematologic System: Denies anemia, easy bruising or bleeding, lymph node enlargement, history of DVT/PE
Endocrine system: Denies generalized weakness, polyuria, polydipsia, polyphagia, heat or cold intolerance, goiter, hirsutism
Nervous system: Denies seizures, loss consciousness, sensory disturbances (numbness, paresthesia, dysesthesias, hyperesthesia), ataxia, loss of strength, change in cognition/mental status/memory, weakness (asymmetric)
Psychiatric: Denies depression/sadness (Feelings of helpless, feelings of hopelessness, lack of interest in usual activities, suicidal ideation), anxiety, obsessive/compulsive disorder
DDX:
- STEMI/NSTEMI
- PE
- Dissection
- Tamponade
- Esophageal Rupture
Physical Exam:
General: Pt is alert & oriented x 3, uncomfortable, pale, diaphoretic and anxious
VS:
- BP: 147/100, RA, supine
- T: 36.8 C oral
- HR: 75 BPM
- O2SAT: 96% RA
- RR: 23 breaths/min, no retractions
Physical Exam:
- Skin: clammy, no edema/erythema, ecchymoses
- Head: normocephalic, atraumatic, non-tender to palpation throughout
- Eyes: symmetrical OU; no evidence of strabismus, exophthalmos or ptosis; sclera white; conjunctiva & cornea clear.
- PERRL, EOMs full with no nystagmus
- Red reflex intact OU
- ENMT: mucous membranes moist, pharynx w no erythema, airway patent, no stridor.
- Neck: no tenderness or stiffness
- Respiratory: Lungs CTABL, breath sounds equal bilaterally, no rales, rhonchi or wheezes
- Cardiovascular: Regular S1 and S2 with no murmurs or gallops
- GI: Abd soft, non-distended, no tenderness, no guarding, no rebound, no CVA tenderness
- Back: No Paravertebral tenderness, no midline tenderness, no spasm
- MSK: No deformity, no edema, no tenderness, FROM
- Neuro: Alert. Normal speech, normal tone, normal gait. CN II – XII intact. Muscle strength 5/5 throughout. Sensation intact. Negative Romberg. Negative Pronator drift. Normal finger-nose-finger. No nystagmus.
DDX:
- STEMI/NSTEMI – likely due to patient story and risk factors (Age, family history)
- PE – not likely due to absence of SOB,O2SAT>95%, pain being non-pleuritic, and no history of VTE (Patient’s well’s score is 0)
- Dissection
- Tamponade
- Pneumothorax
- Pneumonia – not very likely due to absence of cough/fever.
- Esophageal Rupture – not likely due to absence of GI Sxs
Nurse hands you his initial ECG. His Troponins are still in the works
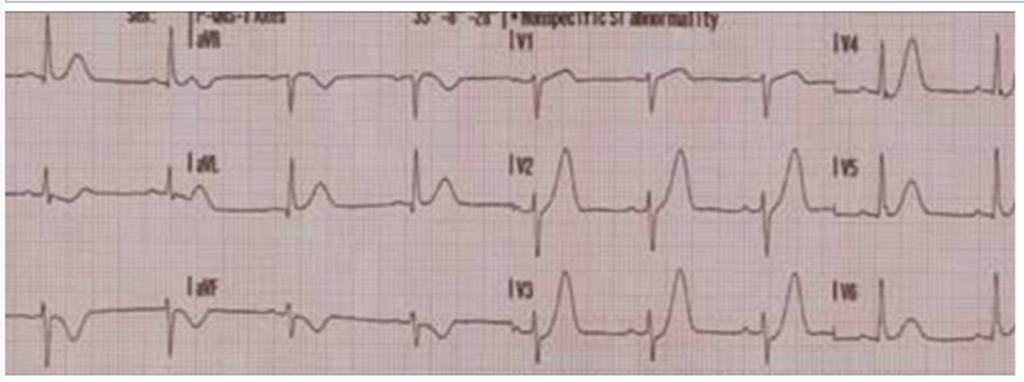
Your actions:
Running to the attending, he tells you these ECG findings are not consistent with MI.
You present the patient, focusing on pertinent findings and insists the attending sees your patient immediately.
Your attending agrees this gentleman is having an MI.
Plan:
- Activate STEMI code – STAT cardiology consult
- IV x 2, Cardiac monitor, pulse ox, Repeat EKG, trend Troponin
- Repeat CXR
- Dual antiplatelet: ASA + Plavix (Clopidogrel)
- Antithrombotic: Heparin
- Statin
- Pain control: Nitroglycerin SL
- Bedside echo to access heart wall movement and aorta
Repeat ECG:
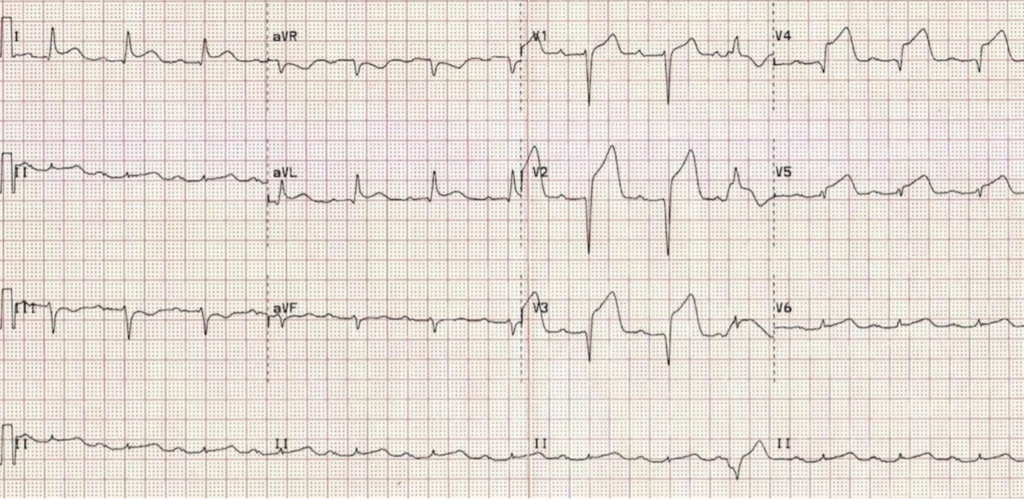
Progress note: Echo revealed no anterior wall movement and intact aorta.
Patient was taken STAT to the Cath lab to which you were allowed to come since this is your patient. 100% LAD occlusion was discovered, and 4 stents were placed. Patient tolerated the procedure well. Patient’s PCP was notified. Patient was set up with a PCP follow up.
Congrats, you just saved someone’s life.


